International Study Finds Thrombectomy Highly Effective Long-Term Treatment for Large Strokes
February 09, 2024
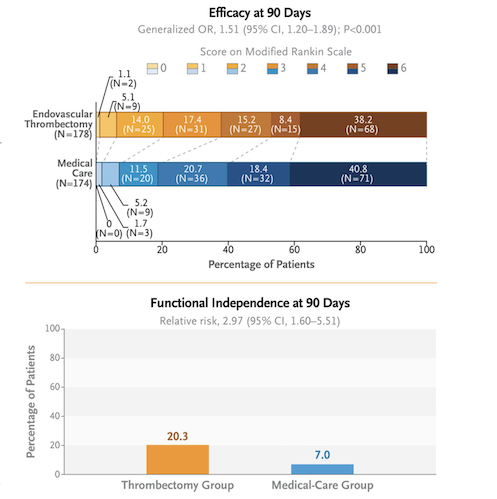
CLEVELAND—In a major, international study, named SELECT2, a University Hospitals (UH) research team found that patients with large strokes had a dramatically better recovery after endovascular thrombectomy plus medical management at long-term follow-up, than patients who only received standard medical management.
Endovascular thrombectomy is mechanical recovery of a clot that is blocking blood flow in an artery. Size of a stroke is determined by the range of damaged brain tissue seen through CT or MRI scans. While thrombectomy has proven effective in smaller strokes, patients with large strokes have been considered too high risk for the procedure.
The SELECT2 study was a tremendous, global team effort, spearheaded by UH as the coordinating center. A total of 352 patients, ages 18 to 85, with large ischemic strokes were randomized at 31 hospitals in North America, Europe, Australia and New Zealand. The primary findings of SELECT2 trial were published last year in the New England Journal of Medicine, demonstrating better clinical outcomes in patients receiving thrombectomy at the 90-day follow-up. Those findings, along with other trials, established efficacy and safety of endovascular thrombectomy in patients with large core strokes.
However, long-term outcomes for these patients were not explored before. As these patients have suffered large strokes, it remains plausible that they will take a longer time to achieve optimal stroke outcomes. The SELECT2 research team opted to address this question and analyzed patient outcomes after one year. The study published today in The Lancet to coincide with its presentation at the International Stroke Conference (ISC 2024) in Phoenix.
Patients receiving thrombectomy procedure demonstrated close to three times higher rates of independent living and twice the rates of independent walking. For every six patients treated, one achieved better outcomes as compared to medical management only. For a comparison, balloon angioplasty for heart attack only benefits one in 20-50 patients. Patients also demonstrated better quality of life scores.
Global Principal Investigator and Lead Author of the study, Amrou Sarraj, MD, said, “Throughout our research and clinical trials over the past three years, we’ve established that endovascular thrombectomy for patients with large ischemic stroke is safe and effective. However, until now, long-term outcomes for these patients remained widely unknown.” Dr. Sarraj is also the Stroke Center and System Director, the George M. Humphrey II Chair in Neurology at University Hospitals, and Professor of Neurology at Case Western Reserve University School of Medicine.
The SELECT2 results represent a major advancement in stroke therapy worldwide, and will bring hope for patients and families in a subgroup of patients who previously would have been thought not to benefit. The study proved that a higher quality of life for these patients persists for at least one year following intervention.
“Now that we have been able to follow these patients for a full year, we have confirmed the long-term benefits of thrombectomy in patients with large core strokes,” Dr. Sarraj explained. “With the evidence that improvement continues, exploration of how we can further improve these outcomes, including efforts on supportive care, such as rehabilitation and adjunctive therapies, becomes very important.”
“University Hospitals is thrilled to have served as the coordinating site for the transformative, international SELECT2 study expanding the indications for thrombectomy in large strokes,” said Daniel Simon, MD, President, Academic & External Affairs, Chief Scientific Officer, and Ernie and Patti Novak Distinguished Chair in Health Care Leadership at University Hospitals. “The results of this study will impact thousands of patients worldwide, significantly improving their quality of life. We look forward to implementing this practice changing treatment for stroke in our health system.” Dr. Simon is also Professor of Medicine and Senior Associate Dean for Academic Affairs at Case Western Reserve School of Medicine.
The study was funded through a grant from Stryker Neurovascular to University Hospitals.
Tags: Clinical trials, Neurology, Stroke, Research


